Flat Panel Detectors (FPD): Principles, Applications, and the New Era of Digital X-ray Imaging
Flat Panel Detectors (FPDs) are essential for converting X-ray signals into high-quality digital images, enabling real-time digital X-ray imaging (DR) across medical diagnostics, industrial non-destructive testing (NDT), and security screening. This article provides a concise yet comprehensive overview of FPDs, covering operating principles, conversion types, medical and industrial applications, key trends, and deployment considerations. The content emphasizes the core terms and developments that influence digital X-ray imaging and low-dose imaging, including indirect conversion, direct conversion, photon-counting, flexible FPD, and AI-assisted imaging.

What is a Flat Panel Detector (FPD)?
An FPD is a detector that converts X-ray radiation into a digital image, typically replacing traditional film with real-time, high-resolution digital imaging capabilities. It acts as the critical signal-readout and conversion stage in the digital imaging chain, directly influencing image processing, diagnostic speed, and radiation dose management.
Indirect vs Direct Conversion
In FPD architectures, two core conversion modes exist, each with trade-offs:
- Indirect conversion: X-ray → scintillator (e.g., CsI) → visible light → photodetector array → TFT readout. Advantage: mature and lower cost; Limitation: spatial resolution affected by light scattering and scintillator performance.
- Direct conversion: X-ray directly interacts with semiconductor material (e.g., amorphous selenium) to create electron-hole pairs, read out via an electric field. Advantage: faster imaging and potentially higher signal-to-noise ratio; Limitation: material purity and manufacturing costs are higher.
In practice, applications weigh speed, dose considerations, and cost. In scenarios demanding very fast imaging or low dose, direct conversion or photon-counting approaches may be preferred; in cost-sensitive contexts, indirect conversion often remains attractive.
Core Operating Principles (Overview)
- Indirect conversion: X-ray → scintillator → visible light → photodetector array → TFT readout → digital image.
- Direct conversion: X-ray → semiconductor → electron-hole pairs → electric-field readout/storage → TFT readout → digital image.
- Common goal: achieve high spatial resolution, low noise, fast imaging, and low radiation dose.
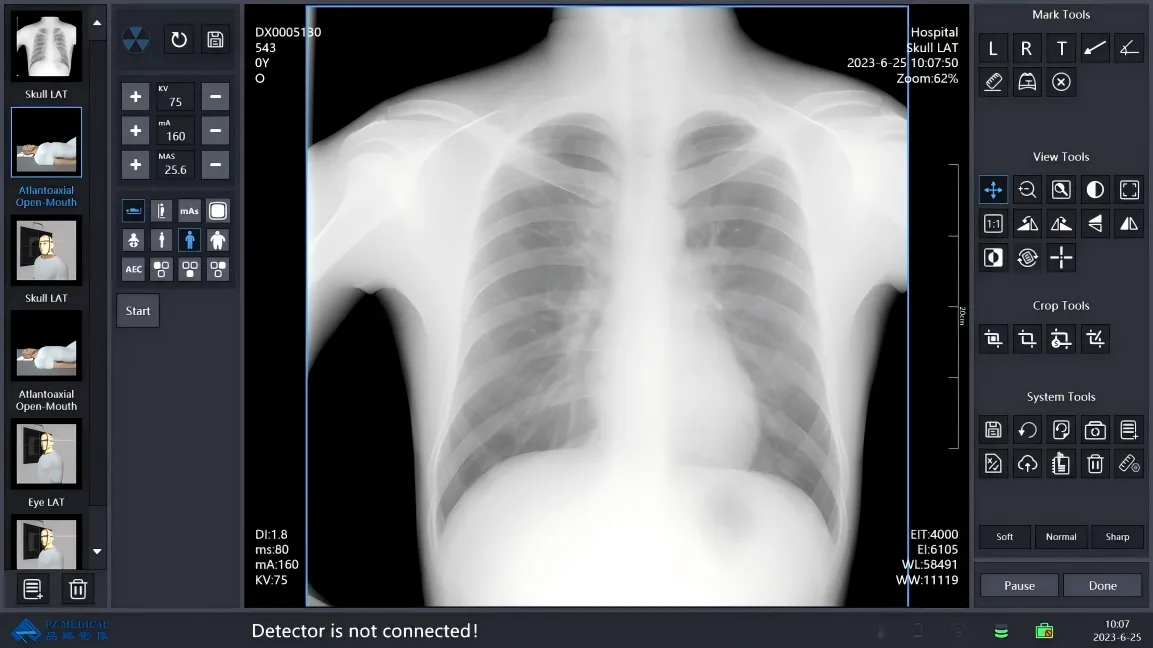
Medical Applications and Value
- Digital Radiography (DR): Improved bone and chest imaging quality and workflow efficiency, reducing patient wait times.
- Digital Mammography (including DBT): High-resolution imaging supports early lesion detection and reduces diagnostic blind spots.
- Interventional Radiology: Real-time imaging aids precise navigation and targeting, enhancing procedural accuracy.
- Image quality and dose management: FP Ds offer significant potential for lowering radiation dose while maintaining or improving diagnostic image quality.
Industrial & Security Applications
- Non-destructive testing (NDT): Detects casting cracks and material defects, improving safety and reliability.
- Electronics inspection: Locates solder joints and circuit anomalies, reducing rework and warranty costs.
- Security imaging: Rapidly identifies items of concern in luggage, improving screening throughput and accuracy.
Frontier Innovations and Trends
- Flexible FPDetectors: Flexible substrates enable imaging on curved and irregular body surfaces, expanding clinical and field use cases.
- AI-Assisted Imaging: AI-based denoising, enhancement, and diagnostic aids improve efficiency and decision consistency.
- Photon-counting: Event-by-event detection promises higher contrast and lower dose; development is advancing and holds strong potential.
- Continued emphasis on low-dose, fast imaging, and scalable deployment across diverse settings.
Technical Challenges and Mitigation
- Indirect conversion: Scattering losses and resolution bottlenecks; mitigation through improved scintillators and lower-noise readouts.
- Direct conversion: Requires high-purity materials and costly manufacturing; mitigation via new materials and scalable production methods.
- Dose-speed-coverage trade-offs: AI-driven optimization, flexible large-area designs, and advanced readout architectures help balance these factors.
Selection and Deployment Guidance
- Clarify application context: medical (DR/DBT/interventional), industrial NDT, or security imaging to determine required frame rate, resolution, and coverage area.
- Conversion type preference: for very fast imaging and low dose, consider direct conversion or photon-counting; for budget-conscious deployments, indirect conversion is often suitable.
- Flexibility needs: for curved anatomy or irregular surfaces, consider a flexible FPD to improve coverage and comfort.
- Imaging software and AI support: prioritize systems with AI-based denoising, automated annotation, and diagnostic assistance.
- Maintenance and cost: consider detector lifespan, system stability, consumables, and upgrade paths.
- Safety and compliance: ensure compliance with radiation safety regulations and dose-monitoring requirements; review clinical/industrial validation data.
For more information, explore the FPD Selection Guide, learn about AI-assisted medical imaging, and review low-dose imaging strategies.
Future Outlook
Flat Panel Detectors are expected to continue advancing toward lower doses, higher resolutions, and faster imaging, with AI and photon-counting driving substantial gains. Flexible and wearable FPDetectors may broaden access to imaging in clinical and field settings, reinforcing the role of digital X-ray imaging as a backbone of medical and industrial diagnostics.
FAQ
- How does FPD differ from CR/RDR?
- FPD is a digital imaging device that directly converts X-ray signals into digital images, enabling real-time imaging and dose efficiency. CR/RDR relies on film or slower digital readout chains, resulting in slower imaging.
- Will the cost of direct conversion hinder adoption?
- Cost is a potential bottleneck, but with advances in materials, manufacturing, and scale, unit costs are expected to decrease, especially in applications requiring high speed and low dose.
- Will AI replace clinicians?
- No. AI serves as an assistive tool to enhance efficiency and consistency; final diagnostic decisions remain the responsibility of clinicians.
References and Further Reading
Refer to field reviews and guidelines from IEEE and other radiology/imaging authorities for deeper technical background, including FP D principles, indirect vs direct conversion, low-dose strategies, and photon-counting applications.
About MAYAMED
This article is prepared by the MAYAMED team. For licensing or reuse, please credit MAYAMED and obtain permission.